Cataract Surgery
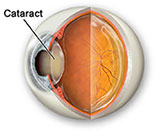
What is a cataract?
A cataract is an opacity or cloudiness in the natural lens of the eye. It is still the leading cause of blindness worldwide and represents an important cause of visual impairment in the United States. The development of cataracts in the adult is related to aging, sunlight exposure, smoking, poor nutrition, eye trauma, systemic diseases, and certain medications such as steroids. A single study has suggested that use of oral vitamin C may help delay the progression of cataracts.
Just as a smudged or dirty camera lens may spoil a photograph, opacity in the natural lens of the eye can result in a blurred image. Patients with cataracts usually complain of blurred vision either at distance, near, or both. This may interfere with tasks such as driving or reading. Other common complaints include glare, halos, and dimness of color vision.
A diagnosis of cataract can only be made by a thorough eye examination including slit lamp (microscopic) evaluation. Other devices are sometimes used to determine if glare interferes with vision. If cataract surgery is being considered, an ophthalmologist will also examine the posterior aspect of the eye, which will include evaluation of the retina and optic nerve. If a cataract is mature (extremely dense) or hypermature (white), an ultrasound device known as a B-scan may be used to rule-out retinal detachment and ocular tumors prior to proceeding with cataract surgery.
The progression of cataracts is highly variable; however, they will invariably worsen in severity. Changing glasses may sometimes be useful in improving vision as the cataract progresses, since cataracts may induce relative nearsightedness. This is the answer as to why some patients with hyperopia (farsightedness) will actually have better vision without glasses in the early stages of cataract development. For most patients, however, changing glasses has minimal impact on overall visual quality. Besides changing glasses, the only other option for treatment of cataracts is cataract surgery.
Cataract Symptoms and Signs
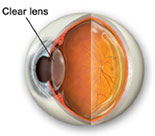
Cataracts are a progressive condition in which the lens of the eye becomes cloudy and grows increasingly opaque. They are usually white, but can be tinted yellow or brown. As a result, the symptoms vary, depending upon the type and severity of the cataract.
When there is only a hint of cloudiness to the lens, the cataract is classified as "trace." As the cloudiness progresses, the cataract may be classified as "mild" to "moderate." Once the cloudiness becomes very pronounced, the cataract is classified as "mature."
As the cataract becomes progressively cloudy, it blurs and distorts vision to an increasing degree. Vision with a cataract is similar to peering through a dirty or frost covered window. As the dirt or frost on the window increases, it becomes more difficult to see a clear image. As the cataract grows more opaque, images become less recognizable. Ultimately, the cataract may become so dense that it blocks light from entering the eye, resulting in needless blindness.
Cataracts are not always white in color. If they assume a yellow or brown tone, they will affect the ways colors appear. This is similar to the way colored lenses in a pair of sunglasses alter colors.
Because cataracts develop at a slow pace, the changes they cause in vision occur slowly. Due to their progressive nature, the symptoms become more pronounced over time.
Common Symptoms
- A gradual deterioration in vision over time
- Objects may appear yellow, hazy, blurred or distorted
- Vision at night or in low light conditions may be dramatically reduced
- Vision in bright light or in the sunshine may be difficult due to glare
- Halos may appear around bright lights at night.
What Causes a Cataract?
The known causes of cataracts include:
- Trauma
- Inflammation inside the eye
- Metabolic abnormalities
- Nutritional deficiencies
- Exposure to various types of radiation
- Use of certain medications
- Genetic predisposition
- Aging
Of these, aging and genetics probably are the most significant factors. There are no known ways to prevent a cataract from developing or to slow the progression of cataract growth.
Cataract Treatment
Initially, vision affected by cataracts can often be improved through either a new glasses prescription or stronger lighting. However, when cataract symptoms affect a person’s ability to do the tasks they want and/or need to do, cataract surgery becomes necessary. In addition, if the level of vision deteriorates too much or if a cataract interferes with the ophthalmologist’s ability to examine the other structures in the back of the eye, cataract surgery may be recommended.
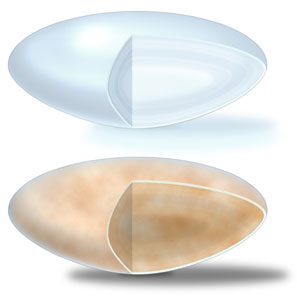
Clear lens (top), Cataract lens (bottom)
The best way to treat cataracts is to remove the cloudy lens and replace it with a new, clear, artificial lens implant. The original cataract will never return. This implant will permanently stay clear and should never have to be replaced. The most advanced technique for this is called phacoemulsification, or phaco. This is the state-of-the-art procedure that we use.
In phaco surgery, a small ultrasonic probe is inserted into the lens of the eye. This probe breaks (emulsifies) the cloudy lens into tiny pieces and gently sucks (aspirates) those pieces out of the eye. Phaco requires a small incision of only 3.0 millimeters or less. Although lasers are being developed for removal of some cataracts, they are not very effective and have a very limited use. At this time, phaco remains the procedure of choice.
Anesthesia
Two types of anesthesia, local or topical, are used in most cataract cases. The most advanced technique, and our preference, is to use topical anesthesia which is administered by placing drops on the surface of the eye. This is the safest method and allows the eye to heal quicker. It eliminates any sensation of pain, but does not prevent your eye from moving around. The second technique, local anesthesia, uses an injection to eliminate any sensation and prevents movement of the eye during surgery. Unfortunately, there is a significant risk with this technique of puncturing the eye. Both types of anesthesia leave you awake during the operation.However, patients are given a relaxing medicine during the operation to make the surgery even more comfortable.
Incision

Phacoemulsification probe
used to break up and remove cataract lens
In order to remove the cataract and replace it with a new lens, we make a microscopic incision in your eye. Where the incision is made depends on the technique your surgeon chooses for you.
Incisions can be made in either of two places in your eye - clear cornea or the sclera. The cornea is the transparent area of your eye over the iris and the pupil. The sclera is often referred to as the white part of your eye.
Our preferred technique is to make a smaller incision in the clear cornea. Smaller incisions usually result in less discomfort during and after surgery, do not require stitches, can aid in reducing astigmatism, and usually provide a faster recovery period
Replacement Lenses
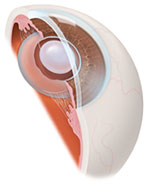
Intraocular lens implant (IOL)
Once the cataract (clouded lens) removal part of the procedure is completed, the doctor will replace it with a permanent, artificial lens called an intraocular lens implant, or IOL.
The most advanced implants are foldable IOLs; lenses can be implanted through the same micro-incision that is created in the phaco procedure. These IOLs are made of a flexible material allowing them to be folded for implantation. Once inside the eye, the lens gently unfolds and returns to its original shape. Several different IOL materials are available today, such as silicone, acrylic, and collamer. All of these materials are biocompatible and there are no cases of a person "rejecting” an implant.
After Your Surgery

IOL in place in eye
One of the benefits of today's small incision cataract procedure is the ability to return home soon after surgery. Before a patient leaves, they will be given written instructions on how to care for their eye, including information on any medications that may be required. Patients can resume normal activities shortly after their surgery.
In time, improvement in vision will continue as the eye recuperates from surgery. The doctor will schedule follow-up appointments, as needed, to check on the visual recovery progress. Most patients will still need glasses for reading following cataract surgery. However, the need for glasses for distance vision may be eliminated following this procedure. In most cases, patients will be healed within two weeks of the surgery and can be given their glasses prescription at that time.
Your Future Vision
Today, advancements in small incision surgery provide the most effective method of restoring vision in the treatment of cataracts. We use the latest state-of-the-art techniques, equipment, and intraocular lenses to provide a safe, fast and effective outcome.
The improvement in vision will not only provide safety and enhance a person’s normal lifestyle and activities, it will also add years of enjoyment to their life. You've got a lot to look forward to!